BPH TREATMENTS
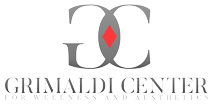
CYSTOSCOPY OR CYSTOURETHROSCOPY
This is a procedure that enables a urologist to view the inside of the bladder and urethra in great detail. It is commonly used to diagnose bladder tumors and identify obstruction of the bladder.
Prior to the procedure, the patient will need to empty their bladder and will then be positioned on an examination table. After administration of local anesthesia, a cystoscope is inserted through the urethra into the bladder. The cystoscope is a thin, lighted tube that is either flexible or rigid. Water or saline is then instilled into the bladder through the cystoscope. As the fluid fills the bladder, the bladder wall is stretched thus allowing detailed viewing by the urologist. Under normal conditions, the bladder wall should appear smooth and the bladder should be normal size, shape and position and there should not be any blockages. If any tissue in the bladder wall appears abnormal, a small sample can be removed through the cystoscope to be analyzed.
The average cystoscopy takes about 5 minutes.
After the cystoscope is removed, the patient’s urethra may be sore and they may feel a burning sensation for up to 48 hours. If discomfort persists, fever develops or urine appears bright red, a physician should be notified.
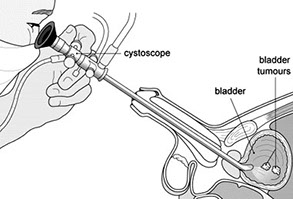
TRANSRECTAL ULTRASOUND/PROSTATE NEEDLE BIOPSY
The prostate is located at the base of the bladder and encircles the urethra like a napkin ring. The prostate provides a portion of ejaculatory fluid, which is important for reproduction. Enlargement of the prostate may cause obstruction of the bladder. The most common indication for a prostate ultrasound (also known as a transrectal ultrasound) is to evaluate men considered at risk for prostate cancer (see prostate cancer screening). Because early prostate cancer cannot be reliably diagnosed by the ultrasound appearance of the prostate alone, the study is usually performed in association with a simultaneous prostate biopsy (see biopsy).
Another common indication for ultrasound is obtaining the volume or size of the prostate for treatment planning purposes. Patients being considered for radioactive seed implantation to treat prostate cancer (brachytherapy) undergo transrectal ultrasound of the prostate to determine prostatic volume. This is necessary to plan the distribution and number of radioactive seeds needed for treatment of the tumor. Transrectal ultrasound may also be performed when transurethral resection of the prostate or thermal therapies of the prostate are planned. Finally, the study is used to determine prostate specific antigen density.
The patient may be asked to use an enema prior to the procedure to better facilitate an adequate examination. The procedure is performed with the patient lying on his side on the examination table.
The ultrasound probe (transducer) is inserted into the rectum to obtain the image of the prostate. Local anesthesia may or may not be used when performing a biopsy. After measuring the prostate volume and identifying any suspicious areas, biopsies are obtained by inserting a special needle through a channel on the transducer. The needle is inserted and the biopsy is obtained quickly. The number of biopsy “cores” obtained is variable but averages six to eight.
The procedure requires 10 to 20 minutes and the main risks are infection and bleeding from the rectum or bladder. Patients are asked to refrain from heavy physical activity for 24 to 48 hours after the procedure. Oral antibiotics are administered prior to and after the biopsy to reduce the likelihood of infection. Some patients may notice blood in their ejaculate for several weeks after the procedure. This is common and not a cause for concern.
Results of the biopsy often take several days. It is important for patients to discuss the results of the biopsy with their urologist. If cancer is diagnosed, a discussion of treatment options is needed. If the biopsy shows no cancer, a strategy for follow up will be discussed. The pathologist may report a precancerous condition on the biopsy that may prompt more frequent follow up or even repeat biopsy.
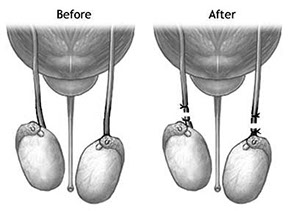
VASECTOMY
This is a minor surgical procedure to cut and close off the tubes (vas deferens) that deliver sperm from the testes; it is usually performed as a means of contraception. The procedure typically takes about 30 minutes and usually causes few complications and no change in sexual function. About 500,000 vasectomies are performed annually in the United States. A vasectomy is less invasive than a tubal ligation (i.e., the procedure used to prevent a woman’s eggs from reaching the uterus) and more easily reversed. An increasing number of couples choose it as a means of permanent birth control.
RENAL/BLADDER/SCROTAL ULTRASOUND
An ultrasound examination, also commonly referred to as a sonogram, is a painless, diagnostic technique that makes use of the behavior of sound waves in the human body. When these sound waves are transmitted into the body, they are reflected in specific ways by specific tissues and organs. These reflected waves can be used to produce images of internal organs without the pain or exposure to radiation. Depending on the reason for the study and the circumstances, ultrasound imaging may be performed in the urologist’s office, in the hospital or in an outpatient facility.
In most cases, very little preparation is needed for an ultrasound examination. Some examinations, such as a bladder scan for residual urine, require limited experience while others, such as ultrasound examinations of the kidneys, testicles or prostate, require more experience or expertise.
The patient will be asked to lie down on the examination table. A clear, water-based gel is applied to the skin over the area to be examined. This gel helps with the transmission of the sound waves. A transducer, which is a hand-held probe, is then moved over that area. Prostate ultrasound examinations are performed by placing a specially designed probe into the rectum. There is no risk of radiation with this study and the patient can resume their daily activities immediately following this test.
MINIMALLY INVASIVE OFFICE TREATMENTS FOR BPH (BENIGN PROSTATIC HYPERPLASIA)
BPH or enlarged prostate is a common condition in men over age 50. An enlarged prostate restricts the flow of urine from the bladder. Dr. Razi performs two in-office Thermotherapies to relieve the symptoms BPH. Thermotherapies are not considered surgical procedures
TUNA® (TRANSURETHRAL NEEDLE ABLATION) THERAPY
Considered being safe, effective and fast. The procedure is performed in an office or outpatient and requires only local anesthesia.
THERMATRX DOT THERAPY
Heat is applied to your prostate with a small, flexible catheter in the urethra. The catheter delivers the exact amount of heat needed to cause long-term symptom relief.
IN OFFICE URODYNAMICS
Urodynamics refers to a group of procedures that are performed to examine voiding (urinating) disorders. The goal of the diagnosis and treatment of these disorders is to both protect the kidneys and keep the patient dry. Any procedure designed to provide information about a bladder problem can be called a urodynamic test. The type of test you take depends on your problem.
Most urodynamic testing focuses on the bladder’s ability to empty steadily and completely. It also can show whether or not the bladder is having abnormal contractions, which cause leakage. Your doctor will want to know whether you have difficulty starting a urine stream, how hard you have to strain to maintain it, whether the stream is interrupted, and whether any urine is left in your bladder when you are done. The urodynamic test is a precise measurement using sophisticated instruments.
FREQUENTLY ASKED QUESTIONS
Yes, there are several surgical options that include procedures that are as minimally invasive as an office treatment to surgery to remove prostate tissue
Currently, we offer microwave therapy, two types of laser surgery, and transurethral resection of the prostate.
The pros of the laser surgeries are that there is a decreased chance of bleeding and the patient typically goes home after the procedure without a catheter. The cons of the laser surgery are that the patient has more burning, frequency and urgency after the procedure than with traditional surgery.
The pros of the TURP or transurethral resection of the prostate is that it is the “gold standard and the post operative flow-rates are better than with the minimally invasive options. There is usually less burning with urination. Also, the patients typically notice the results immediately. The cons of TURP are that there is an increased risk of bleeding, it requires one or more nights in the hospital, and there is an increased risk of urinary incontinence after the procedure as compared with the more minimally invasive procedures.
Usually a patient is back to their normal activity in about a week
Most insurances will cover these procedures